Genital papillomas
Genital papillomas (condylomas) is one of the most common types of sexually transmitted infection.

In this article, we will tell you everything you need to know about genital papillomas – where they come from and how to treat them properly.
Why do genital papillomas appear
The reason for the appearance of such formations on the skin is HPV (human papilloma virus). This virus comes in different types and is in some form in the body of each of us. This especially applies to adults who have sex.
Genital papillomas occur on the genitals of both women and men. Formations are formed on moist tissues in the groin area.
Papillomas on the genitals can be located in the following areas:
◼ vulva;
◼ vaginal walls;
◼ cervix;
◼ between the external part of the genitals and the anus;
◼ back channel;
◼ the tip or shaft of the penis;
◼ scrotum;
◼ anus.
Genital papillomas can also appear on other human mucous membranes – in the mouth or throat.
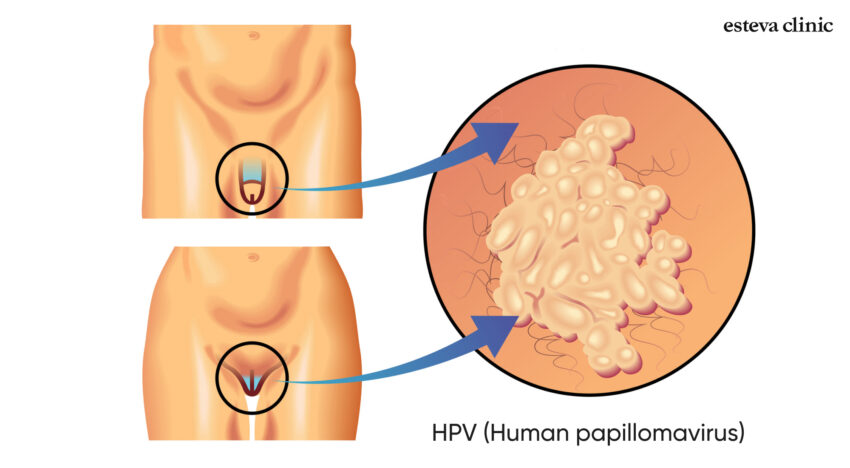
In appearance, these are usually small bumps (often resembling cauliflower in shape) of the same color as the skin. In many cases, formations are so small that it is difficult to notice them with the naked eye.
Some types of HPV can cause acute genital warts or even cancer. Therefore, it is necessary to treat the virus carefully, even though it is in the body of each of us. For example, there are vaccines that can protect against some strains of HPV. If you are regularly bothered by papillomas on the genitals or other parts of the body, you should consult your doctor and learn more about prevention.
How to recognize a papilloma
Faced with such a sensitive topic, people usually want to understand the essence of the problem before going to the doctor. To determine the nature of formations at home, it is necessary to know what features genital papillomas have.
Papillomas on the genitals have a number of symptoms:
◼ the presence of small swellings in the genital area, the color of the swellings may be flesh-colored or different from the color of the skin;
◼ often the shape of the formation resembles a cauliflower inflorescence. This happens due to the close location of several papillomas;
◼ there is itching, burning or other unpleasant sensations on the skin in the genital area;
◼ there may be bleeding during intercourse.

Often, warts are so flat and small that people simply do not pay attention to them. However, in some cases, formations can grow strongly against the background of weakened immunity or due to other individual reasons.
Treatment of genital papilloma
One of the features of genital papillomas is that they can disappear on their own. It depends on the human immune system – if it strengthens and is able to suppress the virus in the body, then the skin manifestations of the virus also disappear.
However, this does not always happen, and if condylomas began to appear regularly, do not disappear and cause discomfort, it is not worth delaying a visit to the doctor.
Which doctor to consult for women and men
If you observe the symptoms of genital papillomas described in the section above, you need to consult a specialist doctor. Depending on the gender of the patient, you need to make an appointment by:
◼ gynecologist, if the symptoms are detected in a woman;
◼ urologist, if unpleasant sensations bother the man.
The doctor conducts a visual examination using a special device – a dermatoscope. Most often, this is enough to determine the nature of the formation.

Dermoscopic view of genital wart
Based on what he saw, the doctor prescribes further tests and then treatment. Among the possible analyses, there may be:
◼ Pap test that allows you to determine cervical cancer. This is a necessary measure, since high-risk HPV can cause oncological diseases;
◼ HPV DNA test is a complex study that helps to identify variants of the virus associated with genital warts. This test, like the Pap test, helps determine the presence of strains capable of causing cervical cancer.
After removing papillomas on the genitals, the doctor can also send the obtained material for a biopsy in order to study the nature of the formation as thoroughly as possible and obtain all the data necessary for a medical conclusion.
Removal of papillomas and condylomas in the clinic
After the doctor has determined the nature of unwanted formations, the optimal method of their removal is prescribed. However, it is important to remember that removing warts from the surface of the skin does not rid a person of HPV. If there is a serious problem inside, then the treatment should be comprehensive and comprehensive.
The following methods are used to remove papillomas on the genitals:
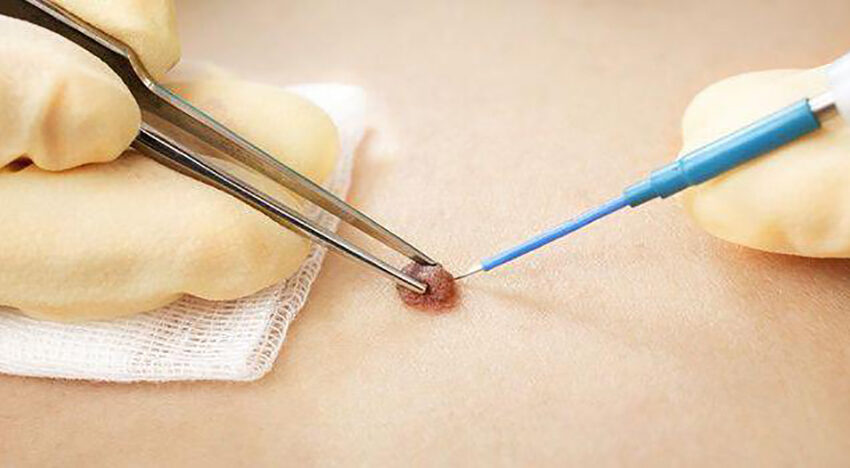
◼ Radio wave electrocoagulation. The electric current converted into radio waves contacts the neoplasm and instantly evaporates it. Visually, it looks like a non-contact incision and sealing of blood vessels. The main advantage of the method is its safety – genital papillomas can be removed almost painlessly, and healing occurs quickly and with minimal risk of scarring. Also, when using this technique, the neoplasm can be sent for histological examination, since radio waves remove only the upper layer of the skin (epidermis). Doctors most often prefer radio wave electrocoagulation, because this method allows more careful control of the depth of removal and removes the formation in one procedure completely, without the need for a repeat procedure.
◼ Removal of papilloma by laser. In the process of applying the technique, the beam destroys tiny blood vessels located inside the papilloma. The procedure is quick and in most cases 1-3 sessions are enough.

◼ Cryotherapy (freezing). Removal of genital warts is carried out with the help of liquid nitrogen, which freezes and thereby removes the formation.
◼ Surgical intervention. If the papillomas do not respond to other treatment methods or are large in size, the doctor may resort to a surgical method of removal. This option is not popular, since the risk of scarring is quite high, and the healing period is longer.
◼ Local treatment with ointments. For milder forms of condyloma, the doctor can prescribe home treatment using ointments, creams or solutions. Such courses usually take several weeks, but do not always have sufficient effectiveness.
Removal of genital warts always begins with an examination by a doctor. The removal itself is usually very quick – removal of one formation takes less than 5 minutes. Before removal, a local treatment is performedanesthesia with ointment or injection. Such a measure helps to reduce all possible pain sensations to a minimum or to avoid them altogether.

Immediately after the removal of the neoplasm, the skin will become smooth and pink, and a crust will form at the very place of removal. It is strictly forbidden to touch or peel it, so as not to provoke the formation of a scar. The crust naturally falls off in 1-3 weeks (depending on the size and location). After that, the skin will gradually return to its normal state. A minimal scar may remain on the surface or there will be no trace at all.
In order to understand which method of removal of formations is best for you, you need to consult a doctor. In one of our videos, we talked about exactly how various skin neoplasms are removed at the Esteva Clinic of Aesthetic Medicine and Dermatology.
If you have any questions or want to make an appointment for an individual consultation with a dermatologist, you can use the “Contact us” or “Contact button” buttons for this. See you at Esteva Clinic!
Видалення папілом на статевих органах
| Назва процедури | Ціна, грн |
|---|---|
| Консультація дерматолога обов’язкова | 790 |
| Контроль після видалення з 30 по 45 день після видалення | Безкоштовно |
| Видалення новоутворень на інтимних зонах | 850 |
| Видалення новоутворень на інтимних зонах від 10 до 20 новоутворень | 4900 |